
Stem Cell Ophthalmology Treatment Study (SCOTS): bone marrow derived stem cells in the treatment of Dominant Optic Atrophy
Introduction
The Stem Cell Ophthalmology Treatment Study (SCOTS) and its subsequent follow on study SCOTS 2, remain the largest stem cell studies for eye disease registered with the National Institutes of Health – www.clinicaltrials.gov Identifier NCT 01920867 and NCT 03011541. Treatments have been performed since November 2012. Both underwent evaluation and approval by an Institutional Review Board. Autologous bone marrow derived stem cells (BMSC) are separated from bone marrow aspirated from the posterior Iliac Crest using minimal manipulation in an FDA cleared class II device. All optic nerve and retinal diseases treated are either progressive or unable to improve spontaneously. SCOTS provides a non-randomized, open label protocol using natural history as the comparator. Neither a placebo nor sham treatment is involved, and all patients accepted into the study receive active BMSC injections.
Detailed inclusion and exclusion criteria have been presented frequently in other published papers and are available on the NIH Clinical Trials website.
Briefly, inclusion criteria include the need to have disease or damage to the optic nerve or retina that is either progressive or unlikely to improve. It must be affecting vision with best corrected acuity of 20/40 or less, or abnormal central or peripheral visual field. Treatment in SCOTS is not available until at least 3 months following any standard disease intervention including surgery, laser or injections. Eye pressures must be well controlled. Patients must be at least 18 years old and medically cleared for anesthesia and surgery.
Exclusion criteria include patients who are not capable or willing to undergo adequate ophthalmologic exam pre- and post-treatment. Patients must be capable of providing informed consent. Patients must not be at serious risk to their general health or visual function if they have the procedure.
Dominant Optic Atrophy (DOA), also known as Autosomal Dominant Optic Atrophy or Kjer’s Optic Neuropathy, is the most commonly diagnosed inherited optic neuropathy (1,2), occurring in 1 in 50,000 individuals (3). OPA loci and genes in the nucleus of human cells code for inner mitochondrial membrane proteins with mutations affecting mitochondrial fusion, Adenosine Triphosphate (ATP) production for cellular energy, control of apoptosis, calcium processing and maintenance of the mitochondrial genome. Approximately 60% of families with DOA exhibit mutations in OPA1(3q28-q29). The patient typically presents with bilateral loss of visual acuity and dyschromatopsia in early childhood. There is a wide variability in visual loss with 13–46% of patients registered as legally blind. The rate of visual loss may be highly variable as well.
Patients are advised to avoid alcohol and tobacco, as well as medications known to interfere with mitochondrial metabolism. Nutritional supplements such as Vitamins B12 and Vitamin D, Coenzyme-Q10, and lutein have been suggested to reduce reactive oxygen induced stress in the optic nerve. Topical neuroprotective or antiapoptotic medications, such as brimonidine, have been tried though evidence of efficacy is anecdotal (3-5).
Methods
Patients enrolling in SCOTS, and presented in this paper, all received a full ophthalmologic examination by the Principal Investigator. This recorded past ocular and medical history, best Snellen and Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuities, slit lamp exam of the eye, intraocular pressure measurement, and fundus evaluation after dilation. Photos of the fundus, Ocular Coherence Tomographic (OCT) and automated perimetry exams were obtained. If suggestion of neovascularization was found on fundus exam, a fluorescein angiogram was performed. Interview with the patient and review of their medical records established the approximate period of compromised vision.
For patients unable to visualize the Snellen 20/400 letter, or largest projected Snellen optotype, vision was evaluated using a 20/200 “E” card from various premeasured distances until the patient reported correctly. Eccentric gaze was permitted to obtain the best possible acuity preoperatively. Vision was recorded as “hand motion” (HM) if the hand-held optotype was not seen at 1 foot but the patient reported perception of hand motions. If the ETDRS visual acuity was less than 5/200, patients were evaluated for their ability to see hand motions. Acuity of eyes which could only perceive light was recorded as “light perception” (LP). If no light could be perceived with the brightest light, vision was stated as “no light perception” (NLP).
Informed consent was carefully and thoroughly obtained for each patient. An extensive discussion of the experimental nature of the intended procedure was provided. All treatments were performed by a single Principal Investigator (JNW) at the same out-patient ambulatory surgical center under anesthesia.
The patients were required to have eye examinations following the procedure at 1, 3, 6 and 12 months post-treatment. The results were to be reported to the Principal Investigator and Study Director.
There are three available treatment arms in the SCOTS protocol. The decision about which arm to provide is based on the degree of visual loss, disease causing visual loss, any potential treatment risk factors and the patient medical status. Both eyes are treated assuming both meet the inclusion criteria. No immunosuppression is utilized as the cells are autologous.
An FDA cleared Class 2 medical device is used to mechanically separate the BMSC concentrate from the bone marrow aspirate. This concentrate has averaged 1.2 billion Total Nucleated Cells including mesenchymal stem cells (MSC) in approximately 14–15 milliliters of concentrate. Retrobulbar injection provides 3 milliliters of BMSC concentrate; subtenons injection provides 1 milliliter of BMSC concentrate; intravitreal injection is 0.05 millimeter; subretinal injection or intra-optic nerve injection is approximately 0.1 milliliter. The remaining concentrate is injected through a 100 micron filter intravenously.
Arm 1 uses stem cell concentrate provided retrobulbar and sub-Tenons followed by intravenous injection.
Arm 2 uses stem cell concentrate provided retrobulbar, sub-Tenon and intravitreal followed by intravenous injection.
Arm 3 treats the eye with better visual acuity using Arm 1 or Arm 2, and the eye with more severe visual acuity impairment a core pars plana vitrectomy followed by subretinal or intra-optic nerve stem cell concentrate. This is followed by intravenous injection. Monocular patients are not eligible for Arm 3.
Patients
Patient 1
A 62-year-old male with a 15-year history of decreased visual acuity secondary to DOA. Genetic testing revealed the presence of the OPA1 gene. Preoperatively, the best corrected visual acuity was 20/80-2 in the right eye (OD) and 20/100-2 in the left eye (OS). The visual acuity on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart was 20/63 OD and 20/100+1 OS. Following informed consent, the patient underwent Arm 2 OU of SCOTS the next day. Eighteen months postoperatively, the visual acuity had improved to 20/40-2 in each eye.
Patient 2
This 39-year-old female was diagnosed with DOA 5 years prior to her inclusion in SCOTS. The preoperative vision was 20/60-1 OD and 20/80+1 OS. The visual acuity on the ETDRS chart was 20/50-2 OD and 20/63+1 OS. Following detailed informed consent, she underwent Arm 2 in each eye. Four months postoperatively she was 20/40 in each eye. Twelve months postoperatively the visual acuity was 20/50 OD and 20/40 OS. The macular thickness OCT improved from 190 to 254 microns and OS from 179 to 254 microns.
Patient 3
This 54-year-old female presented with a visual acuity of 20/200-1 OD and 20/400 OS. Genetic testing was reported as confirming the diagnosis of DOA. The visual acuity on the ETDRS chart was 20/160+2 OD and 20/200+1 OS. She underwent Arm 3 OS and Arm 2 OD as per SCOTS protocol. Two months post-operatively the visual acuity was 20/150 OD and OS. At 6 months OD was 20/100 and OS 20/200 with ETDRS letters 44 OD and 29 OS. At 12 months OD was 20/100-1 and OS 20/250 with ETDRS OD 40.5 letters at 1 meter and OS 31.5 letters at 1 meter.
Patient 4
A 40-year-old female with a 20-year history of visual loss secondary to DOA. The visual acuity was 20/200 in each eye, ETDRS 20/125-2 OU. The patient underwent Arm 2 OU and at 1 month postoperatively the visual acuity was OD 20/150 and OS 20/80. Two months later the patient reported an improvement in color and depth perception. At 6 months postoperatively the visual acuity was OD 20/100-2 and OS 20/150+2. At 9 months the visual acuity was 20/150 OU and at the 1-year postoperative examination the visual acuity was 20/100 OU. The visual fields improved in each eye. At 3 months postoperatively the Visual Field showed OD MD −7.22 P<0.5% PSD 3.54 P<2% with superior arcuate and central/paracentral loss. OS MD −7.82 P<0.5% PSD 6.88 P<0.5% with a dense superior arcuate and central/paracentral scotoma. At the 6 months follow-up examination the visual field in OD improved to MD −5.67 P<1% PSD 2.44 P<5% with the superior arcuate and central/paracentral field loss resolved. OS showed MD −5.87 P<1% PSD 5.25 P<0.5% and the superior arcuate and central/paracentral loss had improved significantly. OCT macular thickness also improved. Preoperatively, the central macular thickness OD was 213 and OS was 173. One month postoperatively the OCT was demonstrated at OD Central 320 Vol Cube 9.6 mm3 thickness um 268, OS Central 239 Vol Cub 8.7 mm3 thickness um 242. A possible mild Epiretinal Membrane (ERM) was noted OU.
Patient 5
This 42-year-old male presented with a 30-year history of visual loss and confirmatory OPA1 testing. The immediate preoperative visual acuity was 20/60-2 OD and 20/70+1 OS, ETDRS 20/80-2 OU. Vision obtained recently by his primary ophthalmologist had been 20/70- OU and stable for several years. The patient underwent Arm 2 OU. Two months postoperatively the visual acuity was 20/60 OD and 20/70+2 OS. At 6 months OD 20/60-2/+1 and OS 20/70-1 with ETDRS OD 20/125 and OS 20/125. At 12 months, the patient’s vision was 20/70- OU with ETDRS 20/100 OU. This was judged to be unchanged because of the historic consistency. Central OCT thickening improved from 247 to 279 OD.
Patient 6
This 43-year-old male with a history of amblyopia OD and a 3-year history of decreased visual acuity OS secondary to DOA presented with a visual acuity of 20/200 OD and 20/400 OS. The patient was positive for OPA1. The ETDRS visual acuity was 20/80-1 OD and 20/200+1 OS. He underwent Arm 2 of the SCOTS protocol and 1 month later patient had improved to OD 20/80 and OS 20/100-. At approximately 4 months post-operatively the patient’s visual acuity was OD 20/80 and OS 20/150+ and it remained stable at the 8-month visit.
Results
Outcomes of 6 patients with DOA treated in the Stem Cell Ophthalmology Treatment Study are presented. Five patients underwent Arm 2 in both eyes and 1 patient underwent Arm 2 in one eye and Arm 3 in the other eye.
Snellen lines of visual acuity were calculated based on LogMAR vision increments as outlined in Table 1 (6). The number of letter improvements assumed 5 letters per Snellen line. Statistical calculations were done assuming both equal variance and unequal variance. A two tailed paired (Dependent). T-test was chosen because the intervention was performed on the same eye. Statistical results were significant at the P<0.001 level for both equal variance and unequal variance (Welch t-test).
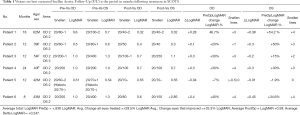
Full table
Of the patients treated, 83.3% (n=5) experienced visual improvements and in all of these cases both eyes improved. Reviewing eyes treated, 83.3% of eyes experienced gains in visual acuity with a median improvement of 2.456 Snellen lines, or approximately 12.29 letters. In LogMAR the average increase in vision was 29.5% and for those eyes that improved, the average increase was 33.3%. The eye undergoing Arm 3 benefited slightly less than eyes treated with Arm 2. In the remaining patient (#5) the visions were potentially minimally decreased when compared to immediate preop vision in the Principal Investigator’s examination lane. However the post-operative visions which were obtained in his primary ophthalmologist’s examination lane were unchanged when compared to preoperative visions obtained in the same lane. Therefore the visions were ultimately judged to be unchanged. This patient had unusually rapid clearing of the intravitreous stem cells which may have meant less time for the BMSC, whether intravitreal or retrobulbar, to provide neuroprotection and mitochondrial transfer.
Discussion
BMSCs have been clinically evaluated in multiple large studies including those involving cardiovascular, neurologic, orthopedic, and ophthalmic diseases. BMSCs have been shown to differentiate into neuron-like cells (7). BMSC have been shown to release neuroprotective compounds including nerve growth factor (NGF) and multiple neurotrophic factors. These can foster the regrowth of axons, protect retinal ganglion cells (RGC) and allow them to integrate into existing neural networks thus re-establishing neural connections (8-10). Autologous treatment with BMSCs preclude immunosuppression, do not result in teratoma formation, and have no ethical or moral objections (11). Though the eye is considered relatively immune privileged, this “privilege” may be compromised in the ocular conditions we are wishing to treat (12), providing an additional benefit of autologous versus embryonic stem cells.
In a glaucoma murine model using BMSC placed in the vitreous cavity, BMSC did not necessarily engraft, but provided a 10–20% increase in the number of surviving RGC (13,14). In a model of optic nerve crush and transection, the use of BMSC provided a doubling of the number of regenerating axons located 100–1,200 µm distal to the lesion site in comparison to a control group. In addition, the survival of RGC improved by 15–28% during the 8–28 days period following the injury (15,16).
In a small clinical study of patients with secondary progressive Multiple Sclerosis (17), the suggestion of a neuroprotective effect was observed following treatment with MSC. These effects were felt to result from either retinal glia activation and glia-mediated neuroprotection or through signaling between the stem cells and the damaged RGCs.
It has been demonstrated that BMSC can differentiate into photoreceptor cells (18), secrete factors to promote photoreceptor survival (19), and have been proven to possess neurotrophic effects on the retina (20,21). We have previously demonstrated the ability of autologous BMSC to successfully treat optic nerve disease (22,23).
Mitochondrial transfer is postulated to be a mechanism by which improvement may be obtained in mitochondrial dysfunction. In a report by Liu et al., MSC were observed using laser scanning confocal microscopy to transfer their mitochondria via a tunneling nanotube-like structure (24). They showed that mitochondrial transfer was frequent and essentially one way from the MSC to endothelial cells, protecting them from apoptosis.
In the one patient with no improvement in vision, the BMSC placed intravitreal per the Arm 2 protocol rapidly cleared and were no longer visible at the 2-month post-operative visit. In our experience it is typical for intravitreal BMSC to persist for approximately 4 months. It is possible their early departure would result in less exosomal release of mRNA and neurotrophic factors, less mitochondrial transfer to the ganglion cell layer on the surface of the retina adjacent to the vitreous and less opportunity for neuronal transdifferentiation and migration into the nerve fiber layer. The result could be an absence of benefit and minimal decrease in vision in one eye as a consequence of residual vitreal debris.
Conclusions
The approach utilized in SCOTS for optic nerve disease provides transfer of the fraction of bone marrow containing BMSC to either the optic nerve directly or to close proximity of the optic nerve and retinal ganglion cell layer.
A number of preclinical studies provide evidence that mitochondrial transfer can take place between BMSC, including MSC, and tissue having undergone injury with the resultant improvement in ATP production allowing for increased survival of the injured cells.
The mechanism of this transfer via a nanotube like structure has been delineated and blockage of this process has been shown to interrupt mitochondrial transfer. Both epithelial and endothelial cells have been shown to accept mitochondria and neural tissue such as the retinal ganglion cell layer and optic nerve are likely capable of participating in this receipt of mitochondria.
Various mechanisms of action have been identified to explain the effects of BMSC. These include secretion of exosomes derived from MSC that release microRNA (miRNA) that enhance the expression of genes promoting cell survival and reduce the actions of harmful genes. Additional exosomes release growth factors including brain-derived neurotrophic growth factor (BDNF), NGF and glial cell line-derived neurotrophic factor (GDNF). BMSC can transfer cytoplasmic structures via cytoplasmic bridges including mitochondria. Immunomodulation is known to occur from BMSC. There are also paracrine effects and the ability of BMSC to transdifferentiate into neurons which provide beneficial effects (25-29).
Diseases affect different layers of the retina and impact the optic nerve and ganglion cells variably. Benefits accrued and the means by which they occur may vary in response to the type of damage detected by the BMSC. One or more mechanism of actions may predominate depending on the disease. Duration of the proximity of BMSC to tissues being treated may be important for these mechanisms to provide positive effects. Mitochondrial transfer appears to be a major contributor to the positive effects of BMSC and therefore a means by which patients with hereditary mitochondrial diseases may improve visual function. Similar patient improvements in our previous report on Lebers Hereditary Optic Neuropathy also suggest that these mechanisms are likely the means to positive effects on the ganglion cell layer and vision (30).
In this paper we presented 6 patients with DOA who underwent treatment in SCOTS with 83.3% of patients and eyes showing visual improvement maintained over a period of up to 24 months. Results showed an average increase in vision of 29.5% on LogMAR. The use of BMSC as provided in the SCOTS study appears to show consistent benefit to vision in mitochondrial optic neuropathies.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Studies are Institutional Review Board approved and reviewed annually and have been registered with the National Institutes of Health: NCT 01920867 and NCT 03011541. Written informed consent was obtained with each patient receiving careful discussion of potential risks, benefits and the experimental nature of the procedure.
References
- Yu-Wai-Man P, Griffiths PG, Chinnery PF. Mitochondrial optic neuropathies - disease mechanisms and therapeutic strategies. Prog Retin Eye Res 2011;30:81-114. [Crossref] [PubMed]
- Lenaers G, Hamel C, Delettre C, et al. Dominant optic atrophy. Orphanet J Rare Dis 2012;7:46. [Crossref] [PubMed]
- Delettre C, Lenaers G, Griffoin JM, et al. Nuclear gene OPA1, encoding a mitochondrial dynamin-related protein, is mutated in dominant optic atrophy. Nat Genet 2000;26:207-10. [Crossref] [PubMed]
- Yu-Wai-Man P, Votruba M, Moore AT, et al. Treatment strategies for inherited optic neuropathies: past, present and future. Eye (Lond) 2014;28:521-37. [Crossref] [PubMed]
- La Morgia C, Carbonelli M, Barboni P, et al. Medical management of hereditary optic neuropathies. Front Neurol 2014;5:141. [Crossref] [PubMed]
- Kim JY, You YS, Kim SH, et al. Epiretinal membrane formation after intravitreal autologous stem cell implantation in a retinitis pigmentosa patient. Retin Cases Brief Rep 2017;11:227-31. [Crossref] [PubMed]
- Dezawa M, Takahashi I, Esaki M, et al. Sciatic nerve regeneration in rats induced by transplantation of in vitro differentiated bone-marrow stromal cells. Eur J Neurosci 2001;14:1771-6. [Crossref] [PubMed]
- Montzka K, Lassonczyk N, Tschöke B, et al. Neural differentiation potential of human bone marrow-derived mesenchymal stromal cells: misleading marker gene expression. BMC Neurosci 2009;10:16. [Crossref] [PubMed]
- Wilkins A, Kemp K, Ginty M, et al. Human bone marrow-derived mesenchymal stem cells secrete brain-derived neurotrophic factor which promotes neuronal survival in vitro. Stem Cell Res 2009;3:63-70. [Crossref] [PubMed]
- Zarzeczny A, Caulfield T. Emerging ethical, legal and social issues associated with stem cell research & and the current role of the moral status of the embryo. Stem Cell Rev Rep 2009;5:96-101. [Crossref] [PubMed]
- Marchetti V, Krohne TU, Friedlander DF, et al. Stemming vision loss with stem cells. J Clin Invest 2010;120:3012-21. [Crossref] [PubMed]
- Johnson TV, Bull ND, Hunt DP, et al. Neuroprotective effects of intravitreal mesenchymal stem cell transplantation in experimental glaucoma. Invest Ophthalmol Vis Sci 2010;51:2051-9. [Crossref] [PubMed]
- Levkovitch-Verbin H, Sadan O, Vander S, et al. Intravitreal injections of neurotrophic factors secreting mesenchymal stem cells are neuroprotective in rat eyes following optic nerve transection. Invest Ophthalmol Vis Sci 2010;51:6394-400. [Crossref] [PubMed]
- Mead B, Logan A, Berry M, et al. Paracrine-mediated neuroprotection and neuritogenesis of axotomised retinal ganglion cells by human dental pulp stem cells: comparison with human bone marrow and adipose-derived mesenchymal stem cells. PLoS One 2014;9:e109305. [Crossref] [PubMed]
- Mesentier-Louro LA, Zaverucha-do-Valle C, da Silva-Junior AJ, et al. Distribution of mesenchymal stem cells and effects on neuronal survival and axon regeneration after optic nerve crush and cell therapy. PLoS One 2014;9:e110722. [Crossref] [PubMed]
- Connick P, Kolappan M, Crawley C, et al. Autologous mesenchymal stem cells for the treatment of secondary progressive multiple sclerosis: an open-label phase 2a proof-of-concept study. Lancet Neurol 2012;11:150-6. [Crossref] [PubMed]
- Kicic A, Shen WY, Wilson AS, et al. Differentiation of marrow stromal cells into photoreceptors in the rat eye. J Neurosci 2003;23:7742-9. [Crossref] [PubMed]
- Inoue Y, Iriyama A, Ueno S, et al. Subretinal transplantation of bone marrow mesenchymal stem cells delays retinal degeneration in the RCS rat model of retinal degeneration. Exp Eye Res 2007;85:234-41. [Crossref] [PubMed]
- Lu B, Wang S, Girman S, et al. Human adult bone marrow-derived somatic cells rescue vision in a rodent model of retinal degeneration. Exp Eye Res 2010;91:449-55. [Crossref] [PubMed]
- Wang S, Lu B, Girman S, et al. Non-invasive stem cell therapy in a rat model for retinal degeneration and vascular pathology. PLoS One 2010;5:e9200. [Crossref] [PubMed]
- Weiss JN, Levy S, Malkin A. Stem Cell Ophthalmology Treatment Study (SCOTS) for retinal and optic nerve diseases: a preliminary report. Neural Regen Res 2015;10:982-8. [Crossref] [PubMed]
- Weiss JN, Levy S, Benes SC. Stem Cell Ophthalmology Treatment Study (SCOTS) for retinal and optic nerve diseases: a case report of improvement in relapsing auto-immune optic neuropathy. Neural Regen Res 2015;10:1507-15. [Crossref] [PubMed]
- Liu K, Ji K, Guo L, et al. Mesenchymal stem cells rescue injured endothelial cells in an in vitro ischemia-reperfusion model via tunneling nanotube like structure-mediated mitochondrial transfer. Microvasc Res 2014;92:10-8. [Crossref] [PubMed]
- Kordelas L, Rebmann V, Ludwig AK, et al. MSC-derived exosomes: a novel tool to treat therapy-refractory graft-versus-host disease. Leukemia 2014;28:970-3. [Crossref] [PubMed]
- Fernández-Messina L, Gutiérrez-Vázquez C, Rivas-García E, et al. Immunomodulatory role of microRNAs transferred by extracellular vesicles. Biol Cell 2015;107:61-77. [Crossref] [PubMed]
- Chen Q, Long Y, Yuan X, et al. Protective effects of bone marrow stromal cell transplantation in injured rodent brain: synthesis of neurotrophic factors. J Neurosci Res 2005;80:611-9. [Crossref] [PubMed]
- Mead B, Berry M, Logan A, et al. Stem cell treatment of degenerative eye disease. Stem Cell Res 2015;14:243-57. [Crossref] [PubMed]
- Huang W, Lv B, Zeng H, et al. Paracrine Factors Secreted by MSCs Promote Astrocyte Survival Associated With GFAP Downregulation After Ischemic Stroke via p38 MAPK and JNK. J Cell Physiol 2015;230:2461-75. [Crossref] [PubMed]
- Weiss JN, Levy S, Benes SC. Stem Cell Ophthalmology Treatment Study (SCOTS): bone marrow-derived stem cells in the treatment of Leber's hereditary optic neuropathy. Neural Regen Res 2016;11:1685-94. [Crossref] [PubMed]
- Holladay JT. Proper method for calculating average visual acuity. J Refract Surg 1997;13:388-91. [PubMed]
Cite this article as: Weiss JN, Levy S. Stem Cell Ophthalmology Treatment Study (SCOTS): bone marrow derived stem cells in the treatment of Dominant Optic Atrophy. Stem Cell Investig 2019;6:41.


